 Cannabis is an annual herbaceous plant (a herb), and cannabinoids are substances for which the human brain seems to be pre-wired. Around 147 million people worldwide, 2.5% of the world population, have used cannabis with no clear evidence of a withdrawal syndrome. As the most widely used illicit substance in the world, cannabis' growing popularity still fills some people with concern about its supposed, potential dangers and, in particular, whether it can actually be addictive.
Cannabis is an annual herbaceous plant (a herb), and cannabinoids are substances for which the human brain seems to be pre-wired. Around 147 million people worldwide, 2.5% of the world population, have used cannabis with no clear evidence of a withdrawal syndrome. As the most widely used illicit substance in the world, cannabis' growing popularity still fills some people with concern about its supposed, potential dangers and, in particular, whether it can actually be addictive.
In August 2015, the International Centre for Science in Drug Policy (ICSDP) launched #CannabisClaims, a campaign by scientists and academics to set the record straight on thirteen of the most oft-repeated claims on cannabis use and regulation, none of which are strongly supported by the scientific evidence. The first debunked claim was that cannabis is addictive as heroin.
 In the past couple of decades, investigators have repeatedly reported that only a relatively small percentage of those who tried cannabis would ever become 'dependent'. Based on a large-scale survey by the United States (US) National Institute on Drug Abuse (NIDA) published in 1994 which asked more than 8,000 people between the ages of 15 and 64 about their use of cannabis and drugs. The researchers found that of those who had tried cannabis at least once, less than 9% eventually fit a diagnosis of cannabis 'dependence'. The corresponding figure for alcohol was 15%; for cocaine, 17%; for heroin, 23%; and for nicotine, 32%. So although cannabis may seem addictive to some, over 91% of those who try it do not get 'hooked'. To put this into perspective, cannabis is less addictive than caffeine and many other legal and illegal substances.
In the past couple of decades, investigators have repeatedly reported that only a relatively small percentage of those who tried cannabis would ever become 'dependent'. Based on a large-scale survey by the United States (US) National Institute on Drug Abuse (NIDA) published in 1994 which asked more than 8,000 people between the ages of 15 and 64 about their use of cannabis and drugs. The researchers found that of those who had tried cannabis at least once, less than 9% eventually fit a diagnosis of cannabis 'dependence'. The corresponding figure for alcohol was 15%; for cocaine, 17%; for heroin, 23%; and for nicotine, 32%. So although cannabis may seem addictive to some, over 91% of those who try it do not get 'hooked'. To put this into perspective, cannabis is less addictive than caffeine and many other legal and illegal substances.  Around the same time as the abovementioned survey an addiction expert at Pennsylvania State University said addiction could generally be defined as "the repeated use of a psychoactive drug which is difficult to stop" and added there might be many explanations for why it was hard to stop, including withdrawal that was too disturbing, or a 'high' that was too enticing. A diagnosis of mild dependence on a psychoactive drug was determined by meeting three of nine criteria; five criteria showed moderate dependence and seven indicated a strong dependence (not all nine applied; e.g., time and effort spent acquiring a substance is a significant feature of heroin addiction, but has no meaning in nicotine addiction and could also be the result of criminalisation, not addiction, but the study authors ignored this. Regardless of what percent of cannabis users can be considered 'dependent', it’s clear that heavy cannabis use is far less damaging than heavy use of heroin, cocaine, methamphetamine or alcohol. Dr Jack E. Henningfield of NIDA and Dr Neal L. Benowitz of the University of California (San Francisco), ranked six substances based on five problem areas (commonly referred to as the Henningfield-Benowitz Ratings):
Around the same time as the abovementioned survey an addiction expert at Pennsylvania State University said addiction could generally be defined as "the repeated use of a psychoactive drug which is difficult to stop" and added there might be many explanations for why it was hard to stop, including withdrawal that was too disturbing, or a 'high' that was too enticing. A diagnosis of mild dependence on a psychoactive drug was determined by meeting three of nine criteria; five criteria showed moderate dependence and seven indicated a strong dependence (not all nine applied; e.g., time and effort spent acquiring a substance is a significant feature of heroin addiction, but has no meaning in nicotine addiction and could also be the result of criminalisation, not addiction, but the study authors ignored this. Regardless of what percent of cannabis users can be considered 'dependent', it’s clear that heavy cannabis use is far less damaging than heavy use of heroin, cocaine, methamphetamine or alcohol. Dr Jack E. Henningfield of NIDA and Dr Neal L. Benowitz of the University of California (San Francisco), ranked six substances based on five problem areas (commonly referred to as the Henningfield-Benowitz Ratings):- Withdrawal: Presence and severity of characteristic withdrawal symptoms.
- Reinforcement: A measure of the substance's ability, in human and animal tests, to get users to take it again and again, and in preference to other substances.
- Tolerance: How much of the substance is needed to satisfy increasing cravings for it, and the level of stable need that is eventually reached.
- Dependence: How difficult it is for the user to quit, the relapse rate, the percentage of people who eventually become dependent, the rating users give their own need for the substance and the degree to which the substance will be used in the face of evidence that it causes harm.
- Intoxication: Though not usually counted as a measure of addiction in itself, the level of intoxication is associated with addiction and increases the personal and social damage a substance may do.
HENNINGFIELD
RATINGS
|
|||||
Substance
|
Withdrawal
|
Reinforcement
|
Tolerance
|
Dependence
|
Intoxication
|
Nicotine
|
3
|
4
|
2
|
1
|
5
|
Heroin
|
2
|
2
|
1
|
2
|
2
|
Cocaine
|
4
|
1
|
4
|
3
|
3
|
Alcohol
|
1
|
3
|
3
|
4
|
1
|
Caffeine
|
5
|
6
|
5
|
5
|
6
|
Cannabis
|
6
|
5
|
6
|
6
|
4
|
1
= Most serious
|
6
= Least serious
|
||||
BENOWITZ
RATINGS
|
|||||
Substance
|
Withdrawal
|
Reinforcement
|
Tolerance
|
Dependence
|
Intoxication
|
Nicotine
|
3*
|
4
|
4
|
1
|
6
|
Heroin
|
2
|
2
|
2
|
2
|
2
|
Cocaine
|
3*
|
1
|
1
|
3
|
3
|
Alcohol
|
1
|
3
|
4
|
4
|
1
|
Caffeine
|
4
|
5
|
3
|
5
|
5
|
Cannabis
|
5
|
6
|
5
|
6
|
4
|
1
= Most serious
|
6
= Least serious
|
||||
*equal ratings
While the scientific evidence weighed in against the contention that cannabis was addictive, there were still a few researchers in the 1990's who were willing to concede the possibility. However, even self-confessed, so-called cannabis 'addicts', who had tried 'Tetrahydrocannabinol (THC) pills' (Marinol), stated that the effect of synthesised THC was more like 5 mg of Valium than actual cannabis and regular users didn’t care for synthetic THC as they basically just got 'knocked down' by it.
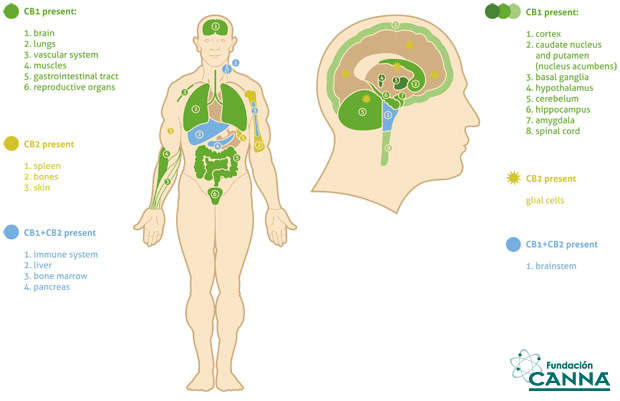
Isolation and structure elucidation of most of the major cannabinoid constituents, including Δ9-tetrahydrocannabinol (Δ9-THC), which is the principal psychoactive molecule in Cannabis sativa - was achieved in the 1960's and 1970's. It was followed by the identification of two cannabinoid receptors in the 1980's and the early 1990's and by the identification of the endocannabinoids shortly thereafter.
In the late 1980's, a team of researchers at the US National Institute of Mental Health (NIMH) found specific receptors in the brain for cannabinoids in all kinds of mammalian brains. “No other drug we tried will recognise that receptor. Opiates won’t recognise it, nor will amphetamine, or cocaine, PCP, LSD, it’s a very unique receptor, and it’s been conserved in evolution.” These same researchers were struck by the relative density of cannabinoid receptors in the cerebral cortex, and the relative lack of the same receptors in the limbic system.
 Cannabis use, of itself, very rarely causes the kind of violent limbic explosions associated with abuse of alcohol, cocaine and amphetamines. The receptor for cannabis, which is heavily distributed in the cerebral cortex, is as researchers described it, "sort of a high-brow receptor". Even fruit flies appear to have a few cannabinoid receptors, fish and sea urchins too, leaving researchers to puzzle over the evolutionary role played by this ancient psychoactive substance. Of what use is a cannbinoid receptor to a chicken or a trout? “This ... gene must have been present early in evolution”, a paper from Toronto’s Addiction Research Foundation attested, “and its conservation implies that the receptor serves an important biological function.” Or, as a researcher at the University of California summed it up: “Why would we express the receptor at high levels if it just made us stupid?”
Cannabis use, of itself, very rarely causes the kind of violent limbic explosions associated with abuse of alcohol, cocaine and amphetamines. The receptor for cannabis, which is heavily distributed in the cerebral cortex, is as researchers described it, "sort of a high-brow receptor". Even fruit flies appear to have a few cannabinoid receptors, fish and sea urchins too, leaving researchers to puzzle over the evolutionary role played by this ancient psychoactive substance. Of what use is a cannbinoid receptor to a chicken or a trout? “This ... gene must have been present early in evolution”, a paper from Toronto’s Addiction Research Foundation attested, “and its conservation implies that the receptor serves an important biological function.” Or, as a researcher at the University of California summed it up: “Why would we express the receptor at high levels if it just made us stupid?” After determining that cannabinoids increase both tonic and phasic dopamine neurotransmission, investigators began addressing the pharmacological mechanisms involved. Initial studies suggested that cannabinoids might increase nucleus accumbens dopamine concentrations, in part, by binding to the dopamine transporter and thereby decreasing uptake into presynaptic terminals, which would be consistent with the pharmacological mechanism of action of other drugs of abuse, such as cocaine. If cannabinoids increase dopamine concentration by decreasing uptake, however, the width of electrically evoked dopamine release events should increase. Electrically evoked dopamine events result in high concentrations of dopamine that saturate dopamine transporters, thus allowing changes in uptake to be discerned. Cannabinoids failed to alter the width of electrically evoked dopamine release events, thereby showing that cannabinoids do not increase dopamine by decreasing uptake.
After determining that cannabinoids increase both tonic and phasic dopamine neurotransmission, investigators began addressing the pharmacological mechanisms involved. Initial studies suggested that cannabinoids might increase nucleus accumbens dopamine concentrations, in part, by binding to the dopamine transporter and thereby decreasing uptake into presynaptic terminals, which would be consistent with the pharmacological mechanism of action of other drugs of abuse, such as cocaine. If cannabinoids increase dopamine concentration by decreasing uptake, however, the width of electrically evoked dopamine release events should increase. Electrically evoked dopamine events result in high concentrations of dopamine that saturate dopamine transporters, thus allowing changes in uptake to be discerned. Cannabinoids failed to alter the width of electrically evoked dopamine release events, thereby showing that cannabinoids do not increase dopamine by decreasing uptake. Furthermore, dopamine uptake inhibitors typically decrease neural firing of dopamine neurons by activating inhibitory dopamine D2 autoreceptors. Thus, a cannabinoid-induced decrease in dopamine uptake would be inconsistent with a cannabinoid-induced increase in dopamine neural firing. Another possibility is that cannabinoids might directly stimulate dopamine neurons; however, this hypothesis is also unlikely, because of multiple reports that dopamine cell bodies lack cannabinoid CB1 receptors. An alternative model suggests that cannabinoids might increase dopamine release by indirectly disinhibiting dopamine neurons. In support of this model, application of cannabinoids to ventral tegmental area brain slices decreased GABAergic inhibitory post-synaptic currents in a GABAA receptor-dependent manner and failed to increase dopamine neural activity following pre-treatment of GABAA receptor antagonists. Taken together, these data suggest that cannabinoids increase dopamine neural firing by decreasing GABAergic inhibition of dopamine neural activity.
Furthermore, dopamine uptake inhibitors typically decrease neural firing of dopamine neurons by activating inhibitory dopamine D2 autoreceptors. Thus, a cannabinoid-induced decrease in dopamine uptake would be inconsistent with a cannabinoid-induced increase in dopamine neural firing. Another possibility is that cannabinoids might directly stimulate dopamine neurons; however, this hypothesis is also unlikely, because of multiple reports that dopamine cell bodies lack cannabinoid CB1 receptors. An alternative model suggests that cannabinoids might increase dopamine release by indirectly disinhibiting dopamine neurons. In support of this model, application of cannabinoids to ventral tegmental area brain slices decreased GABAergic inhibitory post-synaptic currents in a GABAA receptor-dependent manner and failed to increase dopamine neural activity following pre-treatment of GABAA receptor antagonists. Taken together, these data suggest that cannabinoids increase dopamine neural firing by decreasing GABAergic inhibition of dopamine neural activity.
Thus the way cannabis increases dopamine, through separate pathways to addictive substances, is why cannabis is not addictive. Cannabis is not a Dopamine Reuptake Inhibitor (DRI) in the way that cocaine, alcohol (0.2% less addictive than cocaine), methylphenidate (Ritalin) or dexamphetamines ('Dexies') are; they are all addictive DRI's.
"The addicted brain is distinctly different from the non-addicted brain,” wrote Alan Leshner, Former Director at NIMH and NIDA in 2010. “Changes in brain structure and function is what makes it, fundamentally, a brain disease. A metaphorical switch in the brain seems to be thrown as a result of prolonged drug use.” Addiction is both a cause and a consequence of these fundamental alterations in brain function. If physical abnormalities in the brain are at the root of the problem, then any treatment program worth its weight ought to be dealing - directly or indirectly - with these differences in brain state. Writing in the Lancet, researcher Charles O’Brien suggested a similar orientation: “Addiction must be approached more like other chronic illnesses - such as diabetes and chronic hypertension - than like an acute illness, such as a bacterial infection or a broken bone." All of this suggests that we are not likely to win a war on drugs, achieve zero tolerance, or become chemical-free any time soon. The drug problem is an artefact of the basic design of the mammalian brain. Humankind is extraordinarily susceptible to drug abuse anywhere and everywhere certain drugs are widely available - and all because of a 'design quirk' in the reward pathways of the central nervous system.
Way back in 1938, drug policy in Australia was firmly in the hands of the medical profession. A decade before, in 1926, the report of the Rolleston Committee had addressed the problems of opiate addiction and drugs policy. Dominated by doctors, it opted for the medical definition of addiction. Addicts were defined, not as the ‘dope fiends’ of the popular press, but as "a person who, not requiring the continued use of the drug for relief of the symptoms of organic disease, has acquired, as a result of repeated administration, an overpowering desire for its continuance, and in whom withdrawal of the drug leads to definite symptoms of mental or physical distress or disorder". Addiction was seen as a disease, not as a vicious, criminal indulgence and was treated as such.
Way back in 1938, drug policy in Australia was firmly in the hands of the medical profession. A decade before, in 1926, the report of the Rolleston Committee had addressed the problems of opiate addiction and drugs policy. Dominated by doctors, it opted for the medical definition of addiction. Addicts were defined, not as the ‘dope fiends’ of the popular press, but as "a person who, not requiring the continued use of the drug for relief of the symptoms of organic disease, has acquired, as a result of repeated administration, an overpowering desire for its continuance, and in whom withdrawal of the drug leads to definite symptoms of mental or physical distress or disorder". Addiction was seen as a disease, not as a vicious, criminal indulgence and was treated as such.
These days, the terms 'addiction' and 'dependence' are used interchangeably by some, although experts now favour the term 'dependence'. The current revision of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) changed the substance use disorders section. In earlier versions the term ‘dependence’ was selected over ‘addiction’. The term ‘dependence’, while used in past decades to refer to uncontrolled drug-seeking behaviour, has an alternative meaning; the physiological adaptation that occurs when medications acting on the central nervous system are ingested with rebound when the medication is abruptly discontinued. These dual meanings have led to confusion and may have propagated current clinical practices related to under-treatment of pain, as physicians fear creating an ‘addiction’ by prescribing opioids.
The DSM-5 (released in May 2013) no longer uses the terms substance abuse and substance dependence, rather it refers to a single diagnosis of substance 'use disorder' based on nearly the same criteria combined. A minimum of 2-3 criteria is required for a mild substance use disorder diagnosis, while 4-5 is moderate, and 6-7 is severe. The other major change was to remove the criterion related to legal problems and to add one related to substance craving. Defined as mild, moderate, or severe to indicate the level of severity, which is determined by the number of diagnostic criteria met by an individual. Substance use disorders occur when the recurrent use of alcohol and/or drugs causes clinically and functionally significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school, or home. According to the DSM-5, a diagnosis of substance use disorder is based on evidence of impaired control, social impairment, risky use, and pharmacological criteria.
Diagnostic
and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)
Cannabis
Use Disorder
Marijuana*
is the most-used drug after alcohol and tobacco in the United States.
According to The Substance Abuse and Mental Health Services
Administration (SAMHSA), a branch of the US Department of Health and
Human Services data:
PAbout
20 million people ages 12 and up report using marijuana* during the
past month.
PIn
2013, there were 2.4 million people in that age range who had used
marijuana* for the first time within the past 12 months. People
between the ages of 12 and 49 report first using the drug at an
average age of 18.
PIn
the past year, 4.2 million people ages 12 and up met criteria for a
substance use disorder based on marijuana* use.
Marijuana*’s
immediate effects include distorted perception, difficulty with
thinking and problem solving, and loss of motor coordination.
Long-term use of the drug can contribute to respiratory infection,
impaired memory, and exposure to cancer-causing compounds. Heavy
marijuana* use in youth has also been linked to increased
risk for developing mental illness and poorer cognitive functioning#.
Some symptoms of cannabis use disorder include disruptions in
functioning due to cannabis use, the development of tolerance,
cravings for cannabis, and the development of withdrawal symptoms,
such as the inability to sleep, restlessness, nervousness, anger, or
depression within a week of ceasing heavy use.
#This cherry-picked study from the Indian Journal of Psychiatry in 2011, is but ONE of probably thousands on the topics of cannabis use, mental illness and cognitive functioning. Here's another study, also from 2011, which totally debunks the poorer cognitive functioning claim; Cannabis use and cognitive function: 8-year trajectory in a young adult cohort. It concludes; "Cessation of cannabis use appears to be associated with an improvement in capacity for recall of information that has just been learned. No other measures of cognitive performance were related to cannabis after controlling for confounds." And that's just one such contradictory study. If we go back to the ICSDP and #CannabisClaims, another of the debunked claims is that cannabis use impairs cognitive function. In 'Using Evidence to Talk About Cannabis', the scientists state;
#This cherry-picked study from the Indian Journal of Psychiatry in 2011, is but ONE of probably thousands on the topics of cannabis use, mental illness and cognitive functioning. Here's another study, also from 2011, which totally debunks the poorer cognitive functioning claim; Cannabis use and cognitive function: 8-year trajectory in a young adult cohort. It concludes; "Cessation of cannabis use appears to be associated with an improvement in capacity for recall of information that has just been learned. No other measures of cognitive performance were related to cannabis after controlling for confounds." And that's just one such contradictory study. If we go back to the ICSDP and #CannabisClaims, another of the debunked claims is that cannabis use impairs cognitive function. In 'Using Evidence to Talk About Cannabis', the scientists state;
"Claims about the impact of cannabis use on cognitive functioning are at times accompanied by assertions that use leads to school failure, later unemployment, problems with life satisfaction, and other poor outcomes or psychosocial harms. However, scientists have not been able to remove all other possible explanations, and as such the evidence is weak in clearly establishing associations between cannabis use and these outcomes. It’s also noteworthy that a systematic review of all longitudinal scientific studies on this topic found that the evidence did not support a causal relationship between cannabis use by young people and various psychosocial harms"...
*Marijuana is the term preferred by North Americans, a colloquialism. But the correct term is Cannabis sativa L., or just Cannabis.
Resources;
Substance Abuse Facts-CannabisRelative Addictiveness of Drugs
12 Biggest Myths about Marijuana Debunked
Neuroaddiction: The Reward Pathway
The Origins of Marijuana Prohibition in Australia
The Truth About Pot
The Endocannabinoid System
Early phytocannabinoid chemistry to endocannabinoids and beyond
Pre-treatment with delta 1-tetrahydrocannabinol and psychoactive drugs: effects on uptake of biogenic amines and on behavior
Effects of cannabinoids on catecholamine uptake and release in hypothalamic and striatal synaptosomes)
Cannabinoids Enhance Subsecond Dopamine Release in the Nucleus Accumbens of Awake Rats
Electrophysiological effects of cocaine in the mesoaccumbens dopamine system: studies in the ventral tegmental area
Neuronal localization of cannabinoid receptors in the basal ganglia of the rat
Neuroanatomical relationship between type 1 cannabinoid receptors and dopaminergic systems in the rat basal ganglia
Endocannabinoid release from midbrain dopamine neurons: a potential substrate for cannabinoid receptor antagonist treatment of addiction
Inhibition of GABAergic neurotransmission in the ventral tegmental area by cannabinoids
Lack of response suppression follows repeated ventral tegmental cannabinoid administration: an in vitro electrophysiological study
A Brain on Cannabinoids: The Role of Dopamine Release in Reward Seeking
Addiction and dependence in DSM-V
DSM-5 and Substance Use Disorders: Clinicolegal Implications
DSM-5: An Overview of Changes and Controversies
Gregg Cross
How to screen criteria
Using Evidence to Talk About Cannabis



Your website is terribly informative and your articles are wonderful.www.gohotbox.com
ReplyDeleteLove it, thanks!
ReplyDelete