- Jai in Brisbane, sitting among the MCUA's 'Leaves of Change'
In what politicians in Australia would have you believe was an historic vote, the Australian federal parliament 'legalised' Cannabis for medical and scientific purposes. Health Minister Ley announced in February, 2016: “This is an historic day for Australia and many advocates who have fought long and hard to challenge the stigma around 'medicinal cannabis products' so genuine patients are no longer treated as criminal”. Jai was seen by one of the leading neurologists in Australia, Professor Ingrid Scheffer. Tests uncovered that Jai had a rare combination of three different types of epilepsy: Landau Kleffner Syndrome, Continuous Spike Wave Syndrome, Pseudo Lennox Syndrome, plus autism. Violent physical seizures and unseen seizures were almost constantly damaging his young brain.
 One Australian mother who has long campaigned to give her child a chance to survive the cruellest of afflictions without having to worry about being arrested is Michelle Whitelaw from Brisbane. Michelle has spoken widely about the amazing story of how she had to risk all and go against everything she knew about Cannabis when it became the only hope to save her son’s life. And how his miraculous case has helped change the minds of Australia’s lawmakers. Michelle brought up her five children disapproving of recreational drugs, but when one of the country’s top neurologists confirmed there was nothing more Western medicine could do for her son Jai, 11, Cannabis became their only hope. Terrified she would get a knock on the door from the police and face losing her family, Michelle documented their story meticulously.
One Australian mother who has long campaigned to give her child a chance to survive the cruellest of afflictions without having to worry about being arrested is Michelle Whitelaw from Brisbane. Michelle has spoken widely about the amazing story of how she had to risk all and go against everything she knew about Cannabis when it became the only hope to save her son’s life. And how his miraculous case has helped change the minds of Australia’s lawmakers. Michelle brought up her five children disapproving of recreational drugs, but when one of the country’s top neurologists confirmed there was nothing more Western medicine could do for her son Jai, 11, Cannabis became their only hope. Terrified she would get a knock on the door from the police and face losing her family, Michelle documented their story meticulously.Michelle remembers clearly the moment her life changed forever. It was the 16th of January, 2010; a sweltering sunny afternoon in Melbourne at a family barbecue. Her bubbly, chatty, youngest son Jai, then aged 5, stood chatting to his cousins. Then, without warning, his legs gave way and he collapsed. “For 18 long minutes, he convulsed on the ground”, recalls Michelle. “We called an ambulance. Jai was wired up for EEG tests, given blood tests, brain scans. His condition was pretty unusual. They even spoke with neurologists in the United States”.
“As well as the physical fits, Jai was suffering up to 500 sub-clinical seizures a day. Every three to five seconds his brain was misfiring”, recalls Michelle. “Sometimes he’d drop to the floor, other times he’d get that blank look we came to recognise, or we couldn’t even tell”. Jai’s life was never the same again. He was given a cocktail of 35 tablets. His parents Michelle and Andrew installed cameras, microphones, alarms all over the house. They never left their youngest son alone for a minute.
 “Over the next four years, my husband Andrew and our four children: Lachlan, then 11; Samantha, 15; Emily, 16; and Benjamin, 19; all rallied round their little brother”, says Michelle. “We were in and out of hospital. Brain scans revealed that every time his brain misfired, it was frying his brain, which was slowly shrinking. The helplessness of seeing our little Jai deteriorate impacted each one of us. We lost count of the amount of times we nearly lost him and had to resuscitate his tiny body. I was diagnosed with post traumatic stress disorder (PTSD). Our cheery, chatty child, with a huge vocabulary, able to turn his hand to most musical instruments, was left slurring, stuttering, barely able to walk and talk”. In early 2013, Professor Scheffer had some grave news for the family: all clinical solutions on offer had been exhausted. There was nothing else Western medicine could do to stop their son’s continual decline.
“Over the next four years, my husband Andrew and our four children: Lachlan, then 11; Samantha, 15; Emily, 16; and Benjamin, 19; all rallied round their little brother”, says Michelle. “We were in and out of hospital. Brain scans revealed that every time his brain misfired, it was frying his brain, which was slowly shrinking. The helplessness of seeing our little Jai deteriorate impacted each one of us. We lost count of the amount of times we nearly lost him and had to resuscitate his tiny body. I was diagnosed with post traumatic stress disorder (PTSD). Our cheery, chatty child, with a huge vocabulary, able to turn his hand to most musical instruments, was left slurring, stuttering, barely able to walk and talk”. In early 2013, Professor Scheffer had some grave news for the family: all clinical solutions on offer had been exhausted. There was nothing else Western medicine could do to stop their son’s continual decline. We were told to be prepared for sudden, unexpected death”, says Michelle, bitterly. “It was a dark time. The neurologists had warned that weaning Jai off all his high strength medications would be very difficult and could even kill him. We knew other families with children who had died trying. But the side-effects were almost as heartbreaking as his illness. He’d lost 17 teeth due to calcium deficiency; the steroids had damaged his muscles, even his vocal chords; and he had cataracts like an old man. Jai suffered horrible withdrawal symptoms. But like a drug addict coming back to life, Jai improved. By March 2014, his seizures weren't as frequent or brutal. We had Jai back for eight good months”.
We were told to be prepared for sudden, unexpected death”, says Michelle, bitterly. “It was a dark time. The neurologists had warned that weaning Jai off all his high strength medications would be very difficult and could even kill him. We knew other families with children who had died trying. But the side-effects were almost as heartbreaking as his illness. He’d lost 17 teeth due to calcium deficiency; the steroids had damaged his muscles, even his vocal chords; and he had cataracts like an old man. Jai suffered horrible withdrawal symptoms. But like a drug addict coming back to life, Jai improved. By March 2014, his seizures weren't as frequent or brutal. We had Jai back for eight good months”.Sadly, it did not last. “Then one horrific night in November 2014, Jai’s little body shook with six hours of seizures. We didn’t know what to do. I lay next to him in bed, terrified of what would happen next. When he woke up, Jai had no idea who any of us were. He was wetting himself, choking on food. Doctors said there was nothing more they could offer. We brought Jai back home”. Michelle had created a Facebook page for sharing information with other families affected by epilepsy. Many reported great results using Cannabis Oil (CO). “I’d spoken to hundreds of families around the world. Many had been investigated by the police and had children’s services called in for treating children with Cannabis. But we had no other hope”, insists Michelle. “The more I read, I thought the side effects couldn’t be worse than the drugs we’d weaned Jai off”. The family decided to give Cannabis extracts are a try.
 I phoned a Cannabis farmer recommended by another family with an epileptic child and 24 hours later, it arrived: a bottle of THCa extracted from the whole Cannabis plant”, recounts Michelle, referring to tetrahydrocannabinolic acid, the non-psychoactive biosynthetic precursor to THC. “We kept it refrigerated. The heat of the Australian sun could change its effects. I sat on my couch for two days and wondered what I’d do if it didn’t work. Jai was dying. I wasn’t prepared for Jai or my other children to suffer like this any longer. One thing I knew was I was ready to take my own life and his rather than carry on like this. Jai was slumped in his seat, drooling and having constant seizures”. Despite the legal risk that could land Michelle in prison and her children to foster homes, she started the treatment.
I phoned a Cannabis farmer recommended by another family with an epileptic child and 24 hours later, it arrived: a bottle of THCa extracted from the whole Cannabis plant”, recounts Michelle, referring to tetrahydrocannabinolic acid, the non-psychoactive biosynthetic precursor to THC. “We kept it refrigerated. The heat of the Australian sun could change its effects. I sat on my couch for two days and wondered what I’d do if it didn’t work. Jai was dying. I wasn’t prepared for Jai or my other children to suffer like this any longer. One thing I knew was I was ready to take my own life and his rather than carry on like this. Jai was slumped in his seat, drooling and having constant seizures”. Despite the legal risk that could land Michelle in prison and her children to foster homes, she started the treatment.On the morning of 14 December, 2014, I squirted a syringe with one millilitre of whole plant THCa liquid into his little mouth. Jai looked up at me, it was the first time he made eye-contact with me in a long time. A couple of hours later, I gave him another micro-dose. I waited and watched. And that evening, he looked up at me again. And then he asked, ‘Mum can I go outside?’ I cried”. Was it real? It was impossible not to have doubts. “Did I want him to get better so much that I was imagining things?” Michelle explains, describing her shock. “I hooked his little arm under mine and we walked out and sat on the grass. ‘I’m hungry’, said Jai. The transformation was miraculous. Within 48 hours, I said to my husband, ‘We’ve got Jai back!’”
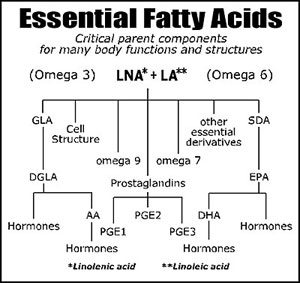
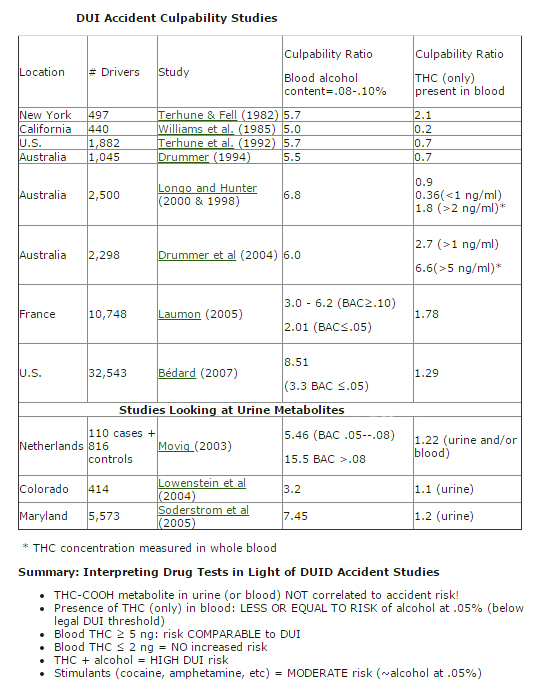
 Last January, just six weeks after Michelle and Andrew had brought Jai home from school and said goodbye to all his friends and teachers for what they all believed was the last time, Jai started school again. “When we took Jai to our local neurologist, she was stunned”, adds Michelle. “Jai told her all about the bicycle he got for Christmas and how he was riding it and enjoyed going to the park. ‘I don't need to know what you're doing’, the neurologist said, ‘but keep doing it’. The last time I’d seen her, I’d asked about medical Cannabis. ‘I can’t support medical Cannabis’, she’d insisted. ‘All I can say, Michelle, is you need to do what you need to do’. Jai has had just four fits in the past 14 months. The theory is we all have cannabinoid receptors linked with all kinds of functions. Jai suffers from a cannabinoid deficiency that can be treated with Cannabis Oils”.
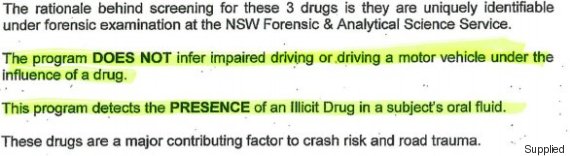
Last January, just six weeks after Michelle and Andrew had brought Jai home from school and said goodbye to all his friends and teachers for what they all believed was the last time, Jai started school again. “When we took Jai to our local neurologist, she was stunned”, adds Michelle. “Jai told her all about the bicycle he got for Christmas and how he was riding it and enjoyed going to the park. ‘I don't need to know what you're doing’, the neurologist said, ‘but keep doing it’. The last time I’d seen her, I’d asked about medical Cannabis. ‘I can’t support medical Cannabis’, she’d insisted. ‘All I can say, Michelle, is you need to do what you need to do’. Jai has had just four fits in the past 14 months. The theory is we all have cannabinoid receptors linked with all kinds of functions. Jai suffers from a cannabinoid deficiency that can be treated with Cannabis Oils”. Despite the incredible recovery, the whole time Michelle admits she was terrified that the family would get a knock on the door from the police and that children services would be informed of her illegal activities. So she began to campaign and travel to meet any local and national health official and politician who would see them and hear Jai’s extraordinary story. “Over the last year, Jai has come with me whenever possible to meet politicians to tell them about his amazing transformation”, says Michelle. “He tells them he can kick a ball now, write, ride a bike and shows them videos on his iPad”. And they appear to have listened. In an historic vote earlier this year, the Australian Parliament voted to pass an amendment to the drug laws to allow farmers to grow and supply Cannabis for medical and scientific purposes. But Michelle has mixed feelings about the 'landmark' legislation. She doubts it will apply to the natural whole-plant Cannabis tincture a grower supplies her son for free.
Despite the incredible recovery, the whole time Michelle admits she was terrified that the family would get a knock on the door from the police and that children services would be informed of her illegal activities. So she began to campaign and travel to meet any local and national health official and politician who would see them and hear Jai’s extraordinary story. “Over the last year, Jai has come with me whenever possible to meet politicians to tell them about his amazing transformation”, says Michelle. “He tells them he can kick a ball now, write, ride a bike and shows them videos on his iPad”. And they appear to have listened. In an historic vote earlier this year, the Australian Parliament voted to pass an amendment to the drug laws to allow farmers to grow and supply Cannabis for medical and scientific purposes. But Michelle has mixed feelings about the 'landmark' legislation. She doubts it will apply to the natural whole-plant Cannabis tincture a grower supplies her son for free.“It's a positive step forward as it means the government has recognised Cannabis as a 'medicinal product'”, said Michelle. “But it's still unlikely to make a difference for families like mine. Each state of Australia needs to adopt the federal legislation changes. People are assuming they can now go to their doctor and grab a script, but there is no supply at present. The changes mean that anyone with a chronic condition should be able to work with their specialists and eventually will have access to pharmaceutical-grade Cannabis, but unless you opt for costly pharmaceutical-grade Cannabis products, families like mine remain criminals”. Michelle says that anecdotally she has heard of mixed results for people with epilepsy in trials of Cannabis-based pharmaceutical products.
“I won't risk Jai on pharmaceutical Cannabis-based medicines when he's seizure-free on the whole plant Cannabis tincture he’s on”, she adds. “It is unclear how the legislation will be implemented, but likely that growers will require a license to grow large cultivations and will have to submit applications. Most compassionate growers here all have criminal convictions. So who ends up being the growers? What experience will they have? Will they be rich businesses who want to make money from the sick and dying with no expertise?” These questions will likely be answered soon.
“It’s a start”, she concludes. “But we still have a long way to go. Still, it’s not that complicated. Jai is 11 years old and gets it. He calls Cannabis ‘my medicine’”.
On 25th of October, 2015, Jai speaks about his wonderful transformation in his own words.
Adapted from, Cannabis Saved My Son's Life